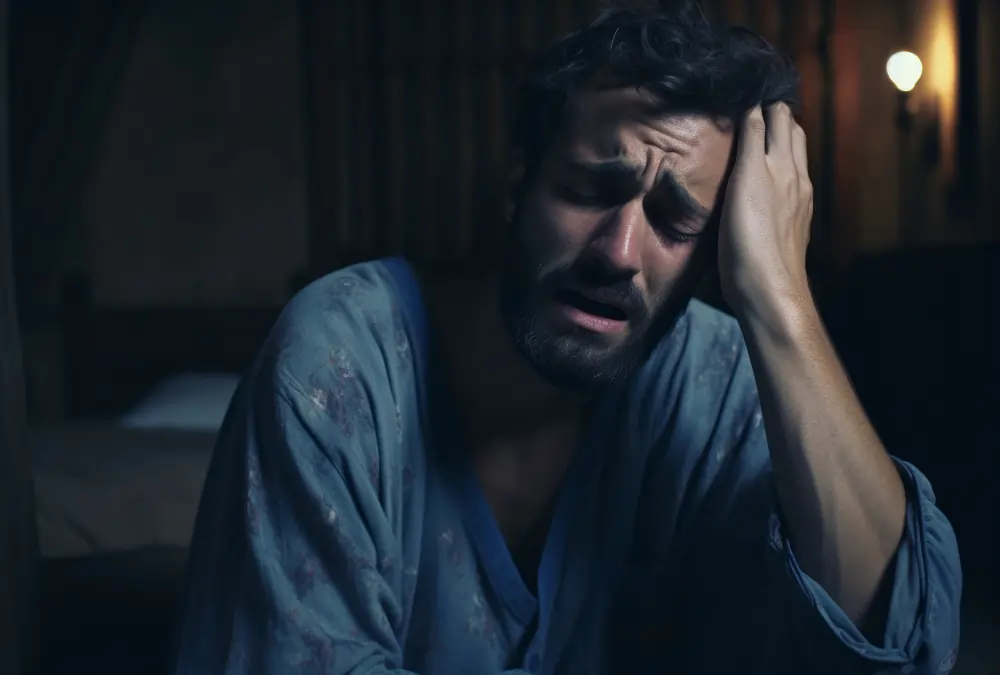
Night sweats can be quite unsettling, especially for individuals already grappling with the challenges of diabetes. The connection between these two can seem enigmatic at first glance. However, in this article, we will unravel the mystery behind diabetic sweats at night. By exploring the topic’s relevance to people with diabetes, we aim to provide valuable insights into the causes and implications of night sweats in this context. So, let’s embark on this intriguing journey to shed light on the phenomenon and offer a deeper understanding for those living with diabetes.
Understanding Night Sweats
Night sweats refer to the occurrence of sudden and excessive sweating during sleep. This phenomenon can affect different parts of the body, such as the underarms, face, neck, hands, and feet. When night sweats strike, they can disrupt sleep patterns, causing frequent awakenings and discomfort. The drenched bed sheets and clothing can be bothersome, leading to a decrease in sleep quality and overall well-being. Dealing with night sweats can be challenging, especially for individuals already managing other health conditions like diabetes. Understanding the causes and potential remedies for night sweats is crucial in order to alleviate their impact on sleep and daily life.
The Diabetes Connection
The link between diabetes and night sweats can be attributed to several factors. One common cause is low blood glucose levels, also known as hypoglycemia. When blood sugar drops too low, it triggers the body to release excess adrenaline, which can lead to sweating during sleep. This adrenaline surge is the body’s way of signaling the need for immediate action to raise blood glucose levels.
In addition to low blood sugar, certain medications used to manage diabetes can also contribute to night sweats. Individuals taking insulin or sulfonylureas, which are common diabetes medications, may experience sweating as a side effect.
It’s important to note that once blood glucose levels return to normal, the night sweats should subside. Proper management of diabetes through medication adjustments, dietary changes, and regular monitoring can help stabilize blood sugar levels, reducing the occurrence of night sweats. Consulting with a healthcare professional is crucial for individuals experiencing persistent or severe night sweats to ensure appropriate diabetes management and to address any underlying concerns.
Types of Sweating Issues in Diabetes

In individuals with diabetes, various types of sweating issues can arise. These include hyperhidrosis, gustatory sweating, night sweats, and sweating due to hypoglycemia.
Hyperhidrosis is characterized by excessive sweating, and in diabetes, it is often caused by the disruption of thermoregulation due to the release of adrenaline. When blood sugar levels drop too low, the body responds by producing excess adrenaline, leading to increased sweating.
Gustatory sweating refers to the phenomenon where eating triggers sweating, particularly in the face, scalp, and neck. This occurs due to nerve damage in the autonomic nervous system, which controls involuntary bodily functions like sweating. In diabetes, this nerve damage can be a result of long-term high blood sugar levels.
Night sweats in diabetes can be attributed to the effect of daytime carbohydrates on thermoregulation. When carbohydrates are consumed during the day, they provide energy for the body. However, at night, when the body’s metabolism slows down, the excess energy from carbohydrates can disrupt thermoregulation and lead to night sweats.
Hypoglycemia, or low blood sugar, is a common cause of sweating in diabetes. When blood sugar levels drop below normal, the body perceives it as a state of emergency and releases adrenaline. This adrenaline surge can trigger sweating as a physiological response to raise blood sugar levels.
Understanding these different types of sweating issues in diabetes is crucial for individuals with the condition. Proper diabetes management, including medication adjustments, lifestyle modifications, and regular monitoring, can help mitigate these sweating issues and improve overall well-being.
Managing Night Sweats
Managing night sweats in diabetes requires a proactive approach. Here are some steps to consider:
1. Monitoring: It is essential to monitor blood sugar levels and symptoms before bedtime. By regularly checking blood sugar levels, individuals can catch low blood sugar early and take appropriate action to prevent night sweats. This can involve using a glucose meter or continuous glucose monitoring system.
2. Simple Carbohydrates: If blood sugar is low before bedtime, consuming a small amount of simple carbohydrates can help raise blood sugar levels. Examples of simple carbs include crackers or a piece of fruit. However, it is important to consult with a healthcare provider or diabetes educator to determine the appropriate amount and timing of these carbohydrates.
3. Consulting Healthcare Provider: Discussing night sweats with a healthcare provider is crucial. They can provide personalized advice, review medication regimens, and make necessary adjustments to manage blood sugar levels effectively. Additionally, they can evaluate any underlying causes or contributing factors to night sweats and address them accordingly.
Remember, managing night sweats in diabetes is a collaborative effort between the individual and their healthcare team. Open communication, regular monitoring, and following the guidance of healthcare professionals are key to effectively managing this symptom and maintaining overall diabetes control.
Conclusion: What Does It Mean When a Diabetic Sweats at Night
We have discussed several types of sweating issues in diabetes, including hyperhidrosis, gustatory sweating, night sweats, and sweating due to hypoglycemia. We explored how adrenaline disrupts thermoregulation, how eating triggers sweating, the impact of daytime carbohydrates on night sweats, and the connection between low blood sugar and sweating.
To manage night sweats effectively, it is important to monitor symptoms before bedtime, catch low blood sugars early, and consult with a healthcare provider for personalized guidance. Additionally, consuming a small amount of simple carbohydrates if blood sugar is low can help raise levels.
Remember, you’re not alone in this sweaty journey. Managing diabetes is about understanding your body and seeking support when needed. Reach out to your healthcare team for assistance, make lifestyle adjustments, and stay proactive in your diabetes management. By taking these steps, you can effectively manage night sweats and improve your overall well-being.
FAQs
Night sweats can be distressing, especially when they disrupt your sleep. If you’re experiencing night sweats due to diabetes, here are some strategies to manage them:
- Blood Glucose Control: Maintaining stable blood sugar levels is crucial. Night sweats often occur when blood glucose levels drop too low. Regular monitoring and adjustments to your diet, exercise, or medications can help prevent this.
- Dress Appropriately: Choose lightweight, breathable fabrics for sleepwear. Cotton sheets are also more breathable, which can help regulate body temperature during the night.
- Cool Sleeping Environment: Keep your bedroom cool by using a fan or adjusting the thermostat. Lighter blankets may also help if you feel hot at night.
- Antiperspirants: Consider using antiperspirants specifically designed for sensitive skin. These can help manage excessive sweating.
- Consult Your Doctor: If night sweats persist, consult your healthcare provider. They can assess your specific situation and recommend personalized strategies to alleviate this symptom.
Yes, high blood sugar levels can indeed cause sweating. Let’s explore the reasons behind this:
- Hyperhidrosis: Excessive sweating, known as hyperhidrosis, can occur due to high blood sugar. Hyperhidrosis isn’t necessarily related to temperature or exercise. It can happen even when you’re not physically active or in a warm environment. When blood glucose levels remain consistently high, it may lead to nerve damage. The nerves that regulate sweat glands become overactive, resulting in increased sweating.
- Autonomic Neuropathy: If you have diabetes and experience sweating along with bladder control problems or an unusual heart rate, it could indicate autonomic neuropathy. This condition arises from nerve damage affecting functions like bladder control, blood pressure, and sweating. Obesity, which often accompanies diabetes, can also contribute to excessive sweating.
- Gustatory Sweating: Gustatory sweating occurs in response to food or eating. People with diabetic autonomic neuropathy or diabetic nephropathy are more likely to experience this type of sweating. If you find yourself sweating profusely in your head and neck region while eating or even just thinking about food, it’s likely gustatory sweating.
- Night Sweats: Night sweats can be caused by low blood glucose levels, especially in individuals taking insulin or sulfonylureas (a type of diabetes medication). When blood glucose drops too low, excess adrenaline is produced, leading to sweating. Once blood glucose returns to normal, the sweating should stop. Other factors, such as menopause, certain types of insulin taken in the evening, and alcohol consumption before bedtime, can also contribute to night sweats.
Yes, night sweats can indeed be a side effect of diabetes. Let’s delve into the details:
- Hypoglycemia (Low Blood Sugar): Night sweats often occur when blood glucose levels drop too low. This is particularly common in individuals taking insulin or certain oral medications for diabetes. When blood sugar falls significantly, the body responds by releasing excess adrenaline, leading to sweating. Once blood glucose returns to normal, the sweating should subside.
- Autonomic Neuropathy: Diabetes can cause nerve damage, including autonomic neuropathy. This condition affects the autonomic nervous system, which controls involuntary functions like sweating, heart rate, and digestion. When the nerves regulating sweat glands become overactive, it can result in excessive sweating, especially at night.
- Gustatory Sweating: Gustatory sweating occurs in response to food or eating. People with diabetic autonomic neuropathy or diabetic nephropathy are more likely to experience this type of sweating. If you find yourself sweating profusely in your head and neck region while eating or even just thinking about food, it’s likely gustatory sweating.
- Other Factors: Besides diabetes itself, other factors can contribute to night sweats:
- Menopause: Women with diabetes may experience night sweats during menopause due to hormonal changes.
- Medications: Some diabetes medications or other drugs can cause sweating as a side effect.
- Alcohol: Consuming alcohol before bedtime can lead to night sweats.
- Obesity: Excess weight can exacerbate sweating, especially if it affects blood sugar control.
Q: Can too much sugar cause night sweats?
Yes, consuming too much sugar can potentially cause night sweats. When your blood sugar levels are high, your body may produce excess sweat in an attempt to cool down, leading to night sweats. Additionally, high blood sugar levels can contribute to dehydration, which can also trigger night sweats. It is important to maintain stable blood sugar levels by following a healthy diet, taking prescribed medications or insulin as directed, and monitoring your blood sugar regularly in order to prevent such symptoms.



 Afrikaans
Afrikaans Albanian
Albanian Amharic
Amharic Arabic
Arabic Armenian
Armenian Azerbaijani
Azerbaijani Basque
Basque Belarusian
Belarusian Bengali
Bengali Bosnian
Bosnian Bulgarian
Bulgarian Catalan
Catalan Cebuano
Cebuano Chichewa
Chichewa Chinese (Simplified)
Chinese (Simplified) Chinese (Traditional)
Chinese (Traditional) Corsican
Corsican Croatian
Croatian Czech
Czech Danish
Danish Dutch
Dutch English
English Esperanto
Esperanto Estonian
Estonian Filipino
Filipino Finnish
Finnish French
French Frisian
Frisian Galician
Galician Georgian
Georgian German
German Greek
Greek Gujarati
Gujarati Haitian Creole
Haitian Creole Hausa
Hausa Hawaiian
Hawaiian Hebrew
Hebrew Hindi
Hindi Hmong
Hmong Hungarian
Hungarian Icelandic
Icelandic Igbo
Igbo Indonesian
Indonesian Irish
Irish Italian
Italian Japanese
Japanese Javanese
Javanese Kannada
Kannada Kazakh
Kazakh Khmer
Khmer Korean
Korean Kurdish (Kurmanji)
Kurdish (Kurmanji) Kyrgyz
Kyrgyz Lao
Lao Latin
Latin Latvian
Latvian Lithuanian
Lithuanian Luxembourgish
Luxembourgish Macedonian
Macedonian Malagasy
Malagasy Malay
Malay Malayalam
Malayalam Maltese
Maltese Maori
Maori Marathi
Marathi Mongolian
Mongolian Myanmar (Burmese)
Myanmar (Burmese) Nepali
Nepali Norwegian
Norwegian Pashto
Pashto Persian
Persian Polish
Polish Portuguese
Portuguese Punjabi
Punjabi Romanian
Romanian Russian
Russian Samoan
Samoan Scottish Gaelic
Scottish Gaelic Serbian
Serbian Sesotho
Sesotho Shona
Shona Sindhi
Sindhi Sinhala
Sinhala Slovak
Slovak Slovenian
Slovenian Somali
Somali Spanish
Spanish Sundanese
Sundanese Swahili
Swahili Swedish
Swedish Tajik
Tajik Tamil
Tamil Telugu
Telugu Thai
Thai Turkish
Turkish Ukrainian
Ukrainian Urdu
Urdu Uzbek
Uzbek Vietnamese
Vietnamese Welsh
Welsh Xhosa
Xhosa Yiddish
Yiddish Yoruba
Yoruba Zulu
Zulu