
Welcome to a comprehensive exploration of one of the most prevalent cardiovascular conditions affecting millions worldwide: Atherosclerosis. In this extensively crafted guide, we delve deep into the symptoms and causes of atherosclerotic disease, shedding light on crucial aspects that underscore the importance of early detection and preventive measures.
1. Unraveling Atherosclerosis: An Overview
Atherosclerosis is the buildup of fats, cholesterol, and other substances in and on the artery walls. This buildup is called plaque. The plaque can cause arteries to narrow, blocking blood flow. The plaque can also burst, leading to a blood clot. This condition, often termed the “silent killer,” manifests insidiously, escalating the likelihood of severe complications if left unaddressed.
2. Identifying Symptoms: Recognizing Early Warning Signs
Chest Pain (Angina)
One of the hallmark symptoms of atherosclerosis, chest pain, or discomfort (angina) arises due to reduced blood flow to the heart muscle. This discomfort can vary from mild to severe, often triggered by physical exertion or emotional stress.
Shortness of Breath
As atherosclerosis impairs blood flow to vital organs, including the lungs, individuals may experience breathlessness, especially during physical activity. This symptom underscores the systemic impact of the disease on respiratory function.
Leg Pain
Peripheral artery disease (PAD), a common manifestation of atherosclerosis, may result in leg pain or cramping during movement. This symptom, known as claudication, highlights the peripheral vascular implications of the disease.
Cognitive Impairment
In advanced stages, atherosclerosis can detrimentally affect cerebral blood flow, leading to cognitive deficits. Individuals may experience memory problems, confusion, or difficulty concentrating, emphasizing the neurological repercussions of this vascular condition.
Hypertension
Elevated blood pressure serves as both a symptom and a risk factor for atherosclerosis. The sustained pressure on arterial walls exacerbates plaque formation, intensifying the cardiovascular burden and necessitating proactive management of hypertension to mitigate complications.
3. Unveiling Causes: Decoding the Pathogenesis of Atherosclerosis
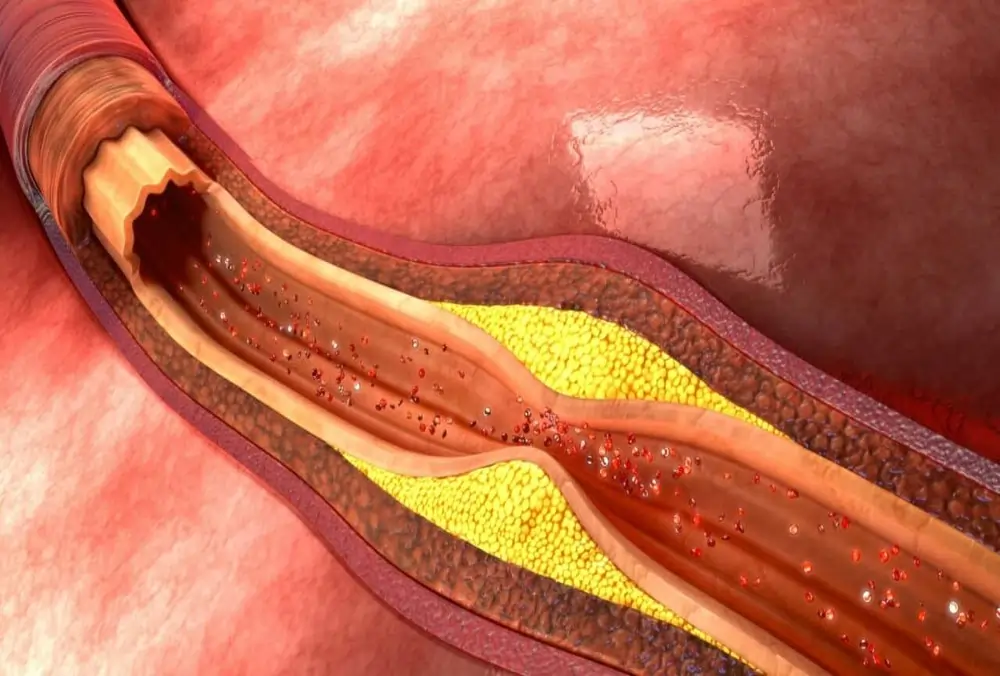
Lipid Accumulation
A primary driver of atherosclerosis, the accumulation of cholesterol-rich lipids within arterial walls initiates the inflammatory cascade that propagates plaque formation. The interplay between circulating lipids and endothelial dysfunction sets the stage for atherosclerotic progression.
Endothelial Dysfunction
Impaired endothelial function, often aggravated by factors like hypertension, smoking, and diabetes, disrupts the delicate balance of vascular homeostasis. This dysfunction paves the way for lipid deposition and the subsequent transformation of arteries into atherosclerotic plaques.
Inflammatory Response
Chronic inflammation serves as a pivotal mediator in atherosclerosis, perpetuating arterial damage and fostering plaque development. The release of cytokines, chemokines, and adhesion molecules orchestrates a pro-inflammatory milieu conducive to atherosclerotic pathogenesis.
Genetic Predisposition
Genetic predispositions play a significant role in predisposing individuals to atherosclerosis. Inherited traits that influence lipid metabolism, inflammatory pathways, or endothelial integrity can markedly impact one’s susceptibility to this cardiovascular disease.
Lifestyle Factors
Modifiable lifestyle factors, including sedentary habits, poor dietary choices, and tobacco use, exert profound influences on atherosclerotic risk. Addressing these behaviors through lifestyle modifications and adherence to healthy practices forms a cornerstone of atherosclerosis prevention and management.
4. Diagnostic Modalities: Navigating Atherosclerosis Evaluation
Non-Invasive Imaging
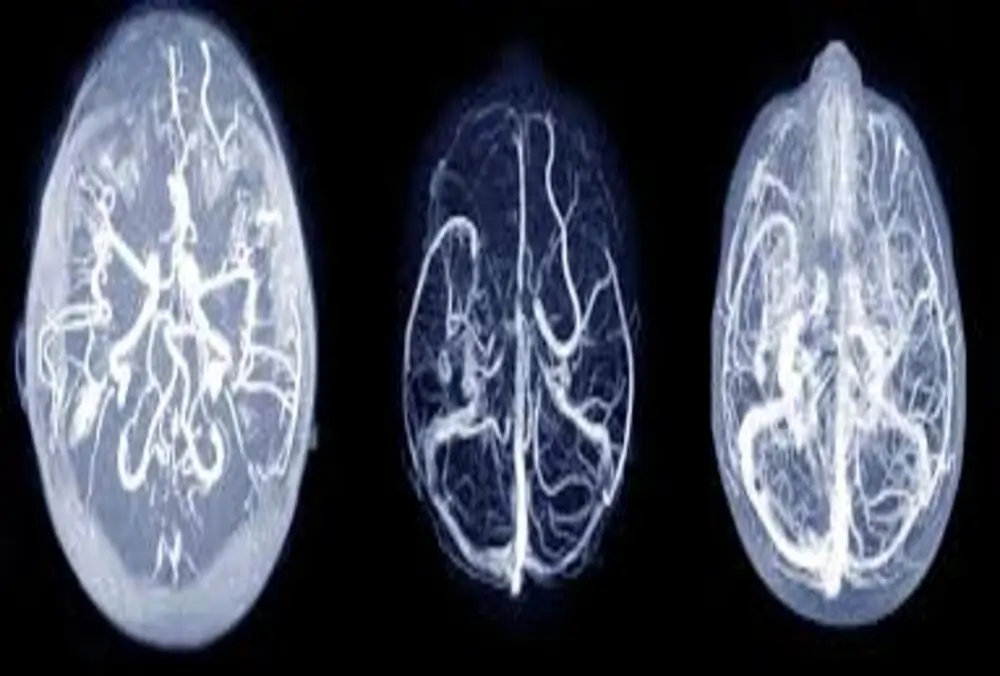
Sophisticated imaging techniques such as ultrasound, CT scans, and MRI facilitate the non-invasive assessment of arterial integrity, plaque burden, and stenotic lesions, enabling precise diagnostic insights into the extent of atherosclerotic involvement.
Blood Tests
Serum biomarkers like lipid profiles, C-reactive protein, and inflammatory markers serve as invaluable tools in gauging cardiovascular risk and monitoring disease progression in individuals with atherosclerosis. Regular blood screenings are integral to comprehensive disease management.
5. Therapeutic Interventions: Promoting Cardiovascular Wellness
Medication Management
Pharmacological interventions, including lipid-lowering agents, antiplatelet therapy, and antihypertensive medications, form the cornerstone of atherosclerosis treatment, aiming to mitigate cardiovascular risks and enhance vascular health through targeted drug regimens.
Lifestyle Modifications
Empowering individuals with knowledge about healthy dietary patterns, regular physical activity, smoking cessation, and stress management equips them with the tools to combat atherosclerosis effectively. Cultivating a heart-healthy lifestyle fosters sustained cardiovascular well-being and reduces disease progression.
Concluding Insights
In conclusion, a comprehensive grasp of atherosclerotic symptoms and causes is imperative in navigating the complexities of cardiovascular health. By fostering awareness, implementing preventive strategies, and embracing a proactive approach to cardiovascular care, individuals can safeguard their well-being and promote longevity free from the shackles of atherosclerotic disease.
FAQs
1. What are the risk factors for developing atherosclerosis?
Atherosclerosis risk factors encompass a wide spectrum, including high cholesterol levels, hypertension, smoking, diabetes, obesity, sedentary lifestyle, and genetic predispositions. Understanding and managing these risk factors is pivotal in mitigating the progression of this cardiovascular condition.
2. Can atherosclerosis be reversed or cured?
While atherosclerosis is a chronic condition, certain lifestyle modifications and medical interventions can help slow disease progression and reduce associated risks. Adopting a heart-healthy lifestyle, adhering to prescribed medications, and undergoing medical treatments as advised by healthcare providers can significantly improve outcomes.
3. How is atherosclerosis diagnosed?
Diagnosis of atherosclerosis involves a combination of clinical evaluations, imaging studies, and laboratory tests. Non-invasive imaging techniques such as ultrasound, CT scans, and MRI, along with blood tests to assess lipid profiles and inflammatory markers, play a crucial role in confirming the presence and extent of atherosclerotic disease.
4. What complications can arise from untreated atherosclerosis?
Untreated atherosclerosis can lead to severe complications, including coronary artery disease, heart attacks, strokes, peripheral artery disease, and even aneurysms. The progressive nature of the disease underscores the importance of timely intervention and comprehensive management to avert potentially life-threatening outcomes.
5. How can one prevent atherosclerosis?
Prevention of atherosclerosis hinges on making proactive lifestyle choices that promote cardiovascular health. Embracing a balanced diet rich in fruits, vegetables, and whole grains, engaging in regular physical activity, avoiding tobacco use, managing stress effectively, and monitoring blood pressure and cholesterol levels are pivotal steps in preventing atherosclerotic progression and safeguarding heart health.


