What is a Blood Glucose Monitoring System?
Living with diabetes requires a vigilant eye on blood glucose levels. This is where a Blood Glucose Monitoring System comes into play, acting as a crucial tool in managing this condition effectively.
Introduction
Living with diabetes is a constant balancing act, and keeping blood glucose levels in check is at the heart of this endeavor. A Blood Glucose Monitoring System (BGMS) plays a pivotal role in this process, offering insights into the fluctuations of blood glucose levels and aiding in making informed decisions regarding diet, medication, and lifestyle choices.
Understanding Blood Glucose
Before delving into the nuances of monitoring systems, let’s understand what blood glucose is. In simple terms, blood glucose, or blood sugar, is the amount of sugar present in your blood. It serves as the primary source of energy for your body’s cells and is derived from the food you consume.
Maintaining blood glucose within a normal range is crucial for overall health. Normal levels vary, but they typically fall between 70 to 140 milligrams per deciliter (mg/dL) before meals and below 180 mg/dL after meals.
The Need for Monitoring

While everyone can benefit from a general awareness of their blood glucose levels, it’s particularly crucial for individuals with diabetes. Diabetes is a condition where the body either doesn’t produce enough insulin (Type 1) or can’t effectively use the insulin it produces (Type 2). Insulin is essential for regulating blood glucose levels, and a disruption in this process can lead to various health complications.
Regular monitoring empowers individuals with diabetes to make timely adjustments to their treatment plans, reducing the risk of hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar), both of which can have severe consequences.
Evolution and Ways of Blood Glucose Monitoring

The evolution of blood glucose monitoring is a fascinating journey marked by significant advancements, transforming the landscape from rudimentary methods to cutting-edge technologies. This progression not only reflects technological innovation but also signifies a substantial improvement in the quality of life for individuals managing diabetes.
Early Days: Urine Testing
In the early stages, urine testing was the primary method for assessing blood glucose levels. This involved analyzing urine samples for the presence of glucose, providing a somewhat indirect measure of blood sugar levels. However, this method lacked precision and real-time insights into glucose fluctuations.
Emergence of Blood Glucose Strips
Advancements led to the introduction of colorimetric blood glucose strips, a more direct approach compared to urine testing. These strips allowed individuals to obtain quicker and more accurate results by testing a small drop of blood. However, this method still had limitations in providing continuous monitoring.
Glucose Sensors Era
The evolution took a significant leap with the advent of glucose sensors. These sensors enabled more frequent and precise monitoring by directly measuring glucose levels in the blood. The transition from strips to sensors marked a substantial improvement in the accuracy and efficiency of blood glucose monitoring.
Continuous Glucose Monitoring (CGM) Revolution
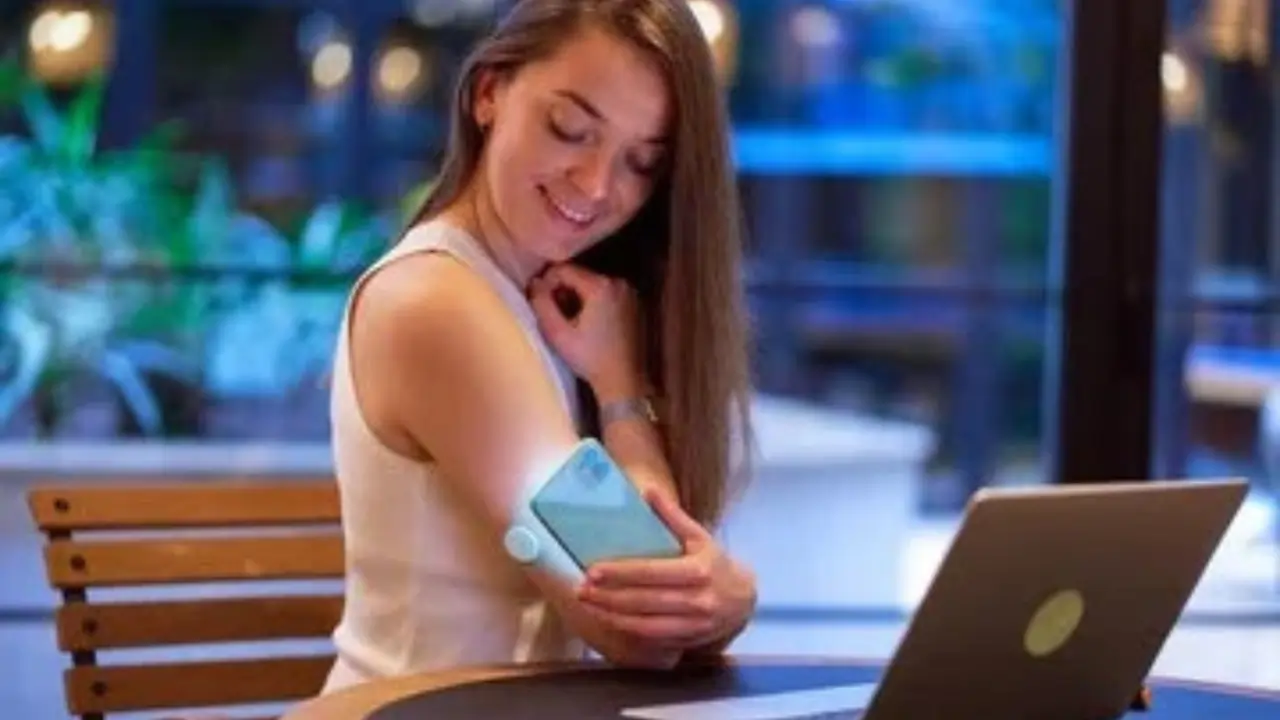
Continuous Glucose Monitoring (CGM) devices represent a pinnacle in blood glucose monitoring evolution. CGM systems offer real-time data by placing a small sensor under the skin, providing individuals with continuous insights into their glucose levels throughout the day and night. This revolutionary technology has significantly enhanced diabetes care, empowering individuals with informed decision-making capabilities.
Recent Technological Advancements
Recent developments continue to push the boundaries of blood glucose monitoring. Integration with smartphones and apps, as well as non-invasive monitoring methods, showcases the commitment to making these technologies more user-friendly and accessible.

In summary, the evolution of blood glucose monitoring reflects a journey from rudimentary methods to the sophisticated, user-centric technologies available today. These advancements not only improve the accuracy of monitoring but also contribute to a higher quality of life for individuals managing diabetes.
How Blood Glucose Monitoring Works?
Understanding how blood glucose monitoring operates is crucial for effective diabetes management. Let’s delve into the detailed processes of Continuous Glucose Monitoring (CGM) and Self-monitoring of Blood Glucose (SMBG), exploring the technologies that empower individuals to monitor and manage their blood sugar levels.
Continuous Glucose Monitoring (CGM) Process and Technology
Continuous Glucose Monitoring employs advanced sensors to measure glucose levels in the interstitial fluid beneath the skin. This process is minimally invasive, involving the insertion of a tiny electrode under the skin. The sensor continuously measures glucose levels throughout the day and night. The collected data is then transmitted to a compact monitor or a smartphone app. Users can not only visualize real-time trends in their glucose levels but also receive timely alerts for high or low blood sugar levels. CGM provides a comprehensive picture of glucose fluctuations, enabling individuals to make informed decisions regarding their diet, medication, and lifestyle.
Self-monitoring of Blood Glucose (SMBG) Process and Devices
Self-monitoring of Blood Glucose, commonly known as SMBG, involves a more traditional yet effective approach. Users prick their fingertips with a lancet, obtaining a small blood sample. This sample is then applied to a test strip and inserted into a glucose meter. The meter swiftly reads the glucose level and displays the result within seconds. SMBG provides a snapshot of blood glucose at a specific moment, aiding individuals in making immediate adjustments to their treatment plan. While it doesn’t offer continuous data like CGM, it remains a reliable method for regular monitoring and is widely accessible.
In summary, the evolution of blood glucose monitoring encompasses both the continuous insights of CGM and the immediate feedback of SMBG, providing individuals with diverse options to manage their diabetes effectively.

Conclusion
In conclusion, a Blood Glucose Monitoring System transcends being a mere tool; it serves as a lifeline for the millions managing diabetes worldwide. The act of regular monitoring is a dynamic and empowering journey, fostering a deep connection between individuals and their health.
Empowering Individuals
Blood glucose monitoring is not just about numbers; it’s about empowering individuals to make informed decisions about their well-being. Through regular monitoring, individuals gain a profound understanding of their body’s responses to various factors such as diet, physical activity, and insulin dosing. This knowledge becomes a powerful tool, enabling them to take proactive measures to maintain optimal blood sugar levels.
Prevention of Complications
The consistent tracking of blood glucose levels acts as a preventive measure against potential complications associated with diabetes. By identifying patterns and trends, individuals can mitigate the risk of both hyperglycemia and hypoglycemia, minimizing the impact on their overall health.
Quality of Life
The impact extends beyond health management; it significantly contributes to a fulfilling life. Individuals equipped with the knowledge gained through monitoring can lead active, vibrant lives, breaking free from the constraints that uncontrolled diabetes may impose. This, in turn, enhances the overall quality of life for those on this diabetes management journey.
In essence, the Blood Glucose Monitoring System becomes a guiding star, illuminating the path towards a healthier, more empowered, and fulfilling life for individuals managing diabetes. Regular monitoring is not just a routine; it’s a beacon of control, resilience, and the promise of a brighter future.
—
FAQs
1. How often should I monitor my blood glucose levels?
Regular monitoring is typically advised, but the frequency may vary. Consult with your healthcare provider for personalized guidance.
2. Can I use CGM if I have a fear of needles?
CGM involves a small sensor under the skin, but it’s less invasive than frequent fingerstick testing. Consult with your healthcare provider to address concerns.
3. Are blood glucose monitoring systems covered by insurance?
Many insurance plans cover the cost of monitoring systems, but coverage varies. Check with your insurance provider for details.
4. Do monitoring systems work for all types of diabetes?
Yes, both CGM and SMBG are applicable to various types of diabetes. Your healthcare provider can help determine the most suitable option for you.
5. Can I share my monitoring data with my healthcare team?
Yes, many monitoring systems allow you to share data with your healthcare provider, fostering collaborative diabetes management.