Introduction
Diabetes mellitus is a common health problem that affects millions of people around the world. When the body doesn’t make enough insulin or can’t use it well, sugar builds up in the blood causing this condition. Insulin plays a key role in helping glucose enter cells to create energy. If there isn’t enough insulin, glucose stays in the blood, leading to many health issues.
Types of Diabetes Mellitus
Several kinds of diabetes mellitus exist each with its causes and traits. These include:
Type 1 Diabetes Mellitus: Type 1 diabetes mellitus is an autoimmune disease where the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. The exact cause of this immune response remains unknown, but genetic or environmental factors might play a role. People with type 1 diabetes mellitus control their blood glucose levels through insulin injections or insulin pumps. This condition affects children and teenagers, but it can start at any age.
Type 2 Diabetes Mellitus: Type 2 diabetes mellitus makes up about 90% of all diabetes cases. This type happens when the body resists insulin’s effects or when the pancreas can’t make enough insulin. Several factors have an impact on Type 2 diabetes mellitus, including lack of exercise excess weight getting older, family genes, and ethnic roots. To manage this type, people might need to change their lifestyle, take pills, or use insulin shots. While adults usually get this type young people can also develop it.
Gestational Diabetes Mellitus: Gestational diabetes affects some women during pregnancy because hormone changes impact how their bodies respond to insulin. This type goes away after giving birth, but it makes women more likely to get type 2 diabetes later on. To manage gestational diabetes, women need to check their blood sugar often, eat healthy foods, exercise, and sometimes take pills or get insulin shots to avoid problems for themselves and their babies.
Other Types of Diabetes Mellitus: A few uncommon forms of diabetes mellitus stem from genetic changes, pancreas problems, infections, drugs, or other underlying causes. These unusual types might show different symptoms and need unique treatment methods compared to the more common forms.
Spotting the Signs
Signs of diabetes mellitus can differ depending on things like the type how bad it is, and how long someone’s had it. Some typical signs include:
- A constant need to drink and pee often
- Always feeling hungry but losing weight for no clear reason
- Feeling tired and weak all the time
- Fuzzy eyesight with headaches
- Hands or feet that feel numb
- Cuts that take forever to heal or getting sick a lot
- Skin that’s dry and itchy
- Trouble getting or keeping an erection, or dryness down there for women
Keep in mind that some people might not show any signs, especially on. That’s why getting your blood sugar checked is key to catching it early.
Possible Health Problems

If not treated or managed well, diabetes mellitus can result in serious and deadly complications, including:
Cardiovascular Diseases: Diabetes mellitus has an impact on the risk of conditions like heart attacks, strokes, angina, and peripheral artery disease. This increased risk stems from harm to the blood vessels and nerves that feed the heart and other key organs.
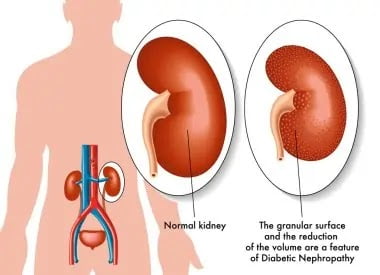
Kidney Disease: Harm to the kidneys called diabetic nephropathy, can lower kidney function or cause complete kidney failure. This can lead to fluid buildup, high blood pressure, and low red blood cell count, and might require dialysis or a new kidney.
Eye Disease: Diabetes can harm the retina, the part of the eye that senses light, which can hurt vision or cause blindness. Also, people with diabetes have a higher chance of getting cataracts, glaucoma, and other eye problems.
Nerve Damage: Diabetes mellitus can cause neuropathy, which has an impact on the body. It results in pain, numbness, or weakness in different body parts the hands and feet. This condition can also harm the function of organs like the digestive system urinary system, and sexual organs.
Foot Complications: Blood vessel and nerve damage to the feet can reduce sensation and blood flow. This leads to a higher chance of infections, ulcers, and in some cases, amputations.
Skin Disorders: Diabetes mellitus can cause skin dryness, itching, cracking, and infections in areas that face friction or pressure.
Susceptibility to Infections: Diabetes mellitus can weaken the immune system making people more likely to get bacterial, viral, fungal, and other infections.
Diagnosing Diabetes Mellitus
To diagnose diabetes mellitus doctors test blood glucose levels when a patient is fasting or after they consume glucose. The World Health Organization (WHO) has set these criteria for diagnosis:
- Fasting plasma glucose (FPG) level ≥ 7.0 mmol/L (126 mg/dL)
- 2-hour plasma glucose (2hPG) level ≥ 11.1 mmol/L (200 mg/dL) after a 75 g oral glucose tolerance test (OGTT)
- Hemoglobin A1c (HbA1c) level ≥ 6.5%
Doctors should run confirmation tests on a different day unless symptoms are clear and blood glucose levels are high. Sometimes, they might need to perform extra tests to figure out the exact type of diabetes mellitus. These could include antibody tests, C-peptide tests, or genetic tests.
Treatment Approaches
The treatment for diabetes mellitus depends on several factors, including the type, severity, and individual considerations. The main goals of treatment are:
To lower and maintain blood sugar levels within the target range
- To handle and regulate symptoms
- To stop or lessen complications
- To boost overall health and wellness
Treatment options may include

Lifestyle Modifications: Making healthy lifestyle changes has a big impact on diabetes management. This includes eating a balanced diet with whole foods watching portion sizes, keeping track of carbs, and staying away from sugary and processed foods. Getting regular exercise is also key to boosting insulin sensitivity, controlling weight, and keeping your heart healthy.
Medications: Doctors prescribe medications to control diabetes mellitus, based on its type and how bad it is. People with type 1 diabetes mellitus need insulin replacement therapy. They might get different kinds of insulin, like rapid-acting short-acting intermediate-acting, or long-acting insulin. People with type 2 diabetes mellitus might take oral medications. These include metformin, sulfonylureas, thiazolidinediones, and dipeptidyl peptidase-4 (DPP-4) inhibitors. These drugs help the body make more insulin or boost insulin sensitivity. Sometimes, doctors might also prescribe shots like glucagon-like peptide-1 (GLP-1) receptor agonists or sodium-glucose cotransporter-2 (SGLT-2) inhibitors.
Insulin Therapy: People with type 1 diabetes mellitus or advanced type 2 diabetes mellitus often need insulin therapy. This treatment involves regular insulin injections or insulin pumps to give the body the insulin it needs throughout the day.
Continuous Glucose Monitoring (CGM): CGM devices can monitor blood glucose levels without interruption. These devices give instant readings and can warn the person about episodes of hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar). CGM systems could make daily blood glucose management better and lower the chance of complications.
Education and Support: Proper education and continuous support play a crucial role for people with diabetes mellitus. Diabetes self-management education (DSME) programs help individuals gain knowledge about their condition, learn blood glucose monitoring techniques, understand how to give insulin or other medications, handle diet and exercise, and avoid or deal with complications. Support groups, counseling, and online resources offer emotional backing and allow people to share experiences and tactics to manage diabetes.
Prevention
Though type 1 diabetes mellitus has no prevention several steps can lower the chances of developing type 2 diabetes mellitus:
Keep your body weight in check: Being overweight increases your chances of getting type 2 diabetes. To lower your risk, eat well, exercise often, and try to reach a healthy weight.
Eat a well-rounded diet: Focus on whole foods, fruits, vegetables lean proteins, and whole grains. At the same time, cut back on processed foods sugary drinks, and too many carbs.
Keep your body moving: Working out boosts how well your body responds to insulin and helps you stay at a healthy weight. Try to do at least 150 minutes of moderate exercise each week, along with some strength training.
See your doctor: Regular check-ups can spot prediabetes or early signs of diabetes. Catching it means you can take action and manage it sooner.
Handle stress well: Long-term stress can mess with your blood sugar levels so it’s key to find good ways to deal with stress. You might try meditating, doing yoga, or spending time on things you enjoy.
Conclusion
Diabetes mellitus is a tricky health problem with different types, signs, effects, and ways to treat it. Learning about it, taking care of yourself, and getting the right medical help can let people with diabetes keep their condition in check and lower the chance of problems. It’s key to team up with doctors to create a treatment plan that fits you and to keep up healthy habits. This helps you control your blood sugar levels and stay healthy overall.
FAQs
Q: What is the difference between diabetes mellitus and diabetes insipidus?
A: Diabetes mellitus is a condition that causes high blood sugar levels due to insufficient or ineffective insulin production or action. Diabetes insipidus is a rare disorder that causes excessive thirst and urination due to a lack of antidiuretic hormone (ADH) or a
reduced response to ADH in the kidneys.
Q: How can I prevent or delay the onset of type 2 diabetes?
A: You can lower your risk of developing type 2 diabetes by making some lifestyle changes, such as losing excess weight, eating a balanced and nutritious diet, exercising regularly, quitting smoking, and limiting alcohol intake. You should also check your blood
glucose levels regularly and consult your doctor if you have any risk factors or symptoms of diabetes.
Q: What are the complications of diabetes mellitus?
A: Diabetes mellitus can lead to serious and sometimes life-threatening complications, such as cardiovascular disease, nerve damage, kidney damage, eye damage, and amputation. These complications can affect various organs and systems in the body and impair their functions. To prevent or reduce the risk of complications, you should follow your treatment plan, monitor your blood glucose levels, and seek medical attention if you notice any signs of problems.
Q: How do I manage my diabetes mellitus during pregnancy?
A: If you have diabetes mellitus before or during pregnancy, you should work closely with your healthcare team to ensure a healthy and safe pregnancy for you and your baby. You may need to adjust your medication, diet, and exercise regimen to keep your blood glucose levels within the target range. You should also have regular prenatal visits and tests to monitor your and your baby’s health and development.
Q: What are the resources and support available for people with diabetes mellitus?
A: Living with diabetes mellitus can be challenging and stressful, but you are not alone. Many resources and support groups can help you cope with your condition and improve your quality of life. You can find information, education, and guidance from various sources, such as your healthcare providers, diabetes educators, nutritionists, pharmacists, and counselors. You can also join online or offline communities, forums, and networks of people with diabetes mellitus who can share their experiences, tips, and advice with you.